When mastitis is identified in a cow’s quarter(s), it is important to identify the pathogen causing the infection because different categories of pathogens require different management strategies. Without a diagnosis, there is no way to know if a given antibiotic will work. However, once you know the infection agent, a dairy farmer can work with his or her veterinarian to target an effective treatment plan. Prudent use of antibiotics reduces the likelihood of resistant pathogens developing and can reduce the duration of treatment a cow may need which decreases operation costs.
The main bacteria responsible for causing mastitis can be divided into two categories: contagious and environmental.
Contagious bacteria
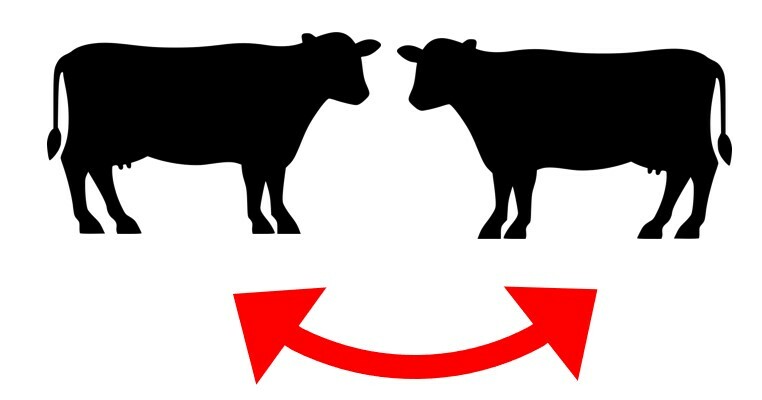
With contagious bacteria, the dairy cow serves as the host and bacteria are transferred from a cow with an infected udder to a healthy cow. The bacteria are often spread cow-to-cow during milking procedures via the milking machine, a milker’s hands or a reused milking towel. Bacterial transfer can also occur from cow-to-cow if milk leakage occurs from the udder into the stall.
The major contagious pathogens include:
- Staphylococcus aureus
- Coagulase-negative staphylococci (CNS)
- Streptococcus agalactiae
- Streptococcus dysgalactiae
- Mycoplasma bovis
- Mycoplasma spp.
- Corynebacterium bovis
Contagious bacteria are mainly Gram-positive mastitis infections. Infected cows usually show abnormal milk and elevated somatic cell count. Gram-positive infections usually respond well to antibiotic treatment. However, symptoms caused by Mycoplasma species are unique in that typically multiple quarters of the animal are infected and it is common for cows to show signs of joint swelling and pain. Most Mycoplasma species do not respond to antibiotic treatment. In fact, for M. bovis, the most common mycoplasma mastitis specie in cattle, there is no treatment.
Prevention involves post-milking teat dip, milk time hygiene, segregation of infected cows and culling of cows with chronic contagious mastitis that are not responsive to treatment.
Environmental bacteria
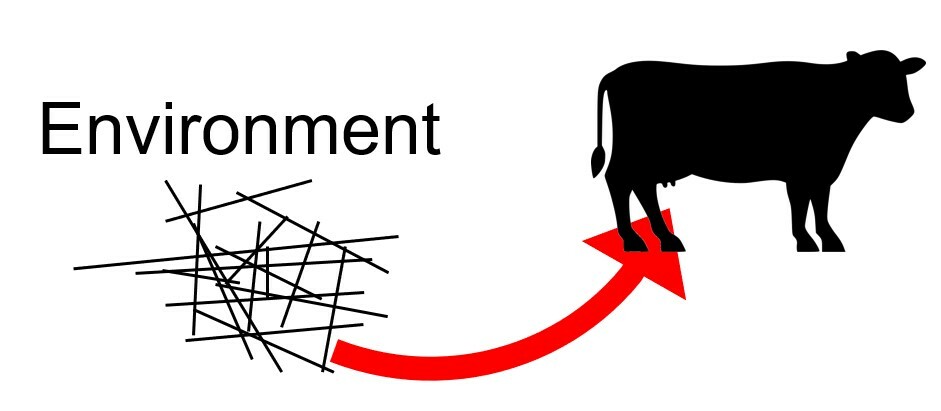
Environmental bacteria are present in the environment including: bedding, soil, walkways, in the pasture or any surface with which the cow or her manure comes in contact. The infection route is from environment to the udder. The environmental bacteria load is highly correlated with the hygiene of the barn and stalls and the cow and udder. Organic materials used for bedding like wood shavings, straw or recycled dry manure solids are common sources of environmental bacteria.
Environmental pathogens are also categorized as Gram-negative mastitis infections. Infected cows tend to get systemically sick and would be considered a “hotter,” more acute case of mastitis.
The major environmental pathogens include:
- Streptococcus uberis
- Streptococcus dysgalactiae
- Some Coagulase-negative staphylococci species
- Escherichia coli
- Klebsiella spp.
- Enterococcus spp.
- Serratia marcescens
- Trueperella pyogenes/P. indolicus
- Yeasts
- Prototheca spp.
- Bacillus spp.
Control of environmental mastitis involves the following recommended management from the Cornell University College of Veterinary Medicine:
- Cow comfort - Provide well designed stalls that are utilized in a correct manner by cattle.
- Provide a clean and dry housing area with adequate bedding that is frequently groomed to remove wet and soiled bedding daily.
- Make sure outside cow areas are clean and well drained. Standing water and muddy areas must be eliminated.
- Be sure to keep cross-over alleys, walkways and areas around waters where cows may congregate clean and free of manure which might splash up on to the udder.
- Make sure barns are well ventilated to limit heat stress and the growth and survivability of bacteria.
- Make sure teats are clean, sanitized, well stimulated and dried prior to attachment of the milking unit.
- Ensure good claw alignment and support during milking. Inflations need to be in good condition to avoid liner slips.
- Be alert to weather conditions (hot and humid) that may initiate an outbreak of environmental mastitis.
- Keep good records and culture all clinical cases to identify the early stages of a mastitis outbreak.
Mastitis-causing Pathogens and Antimicrobial Use
The basic difference in categories of mastitis is their physiology or cell structure.
Gram-positive bacteria have a thick cell wall. The cell wall’s membrane is highly selective about how and what move in and out. The cell wall is attacked by penicillin antibiotics, making Gram-positive bacteria more sensitive to these commonly used types of antibiotics.
Gram-negative bacteria have a thin cell wall sandwiched between two membranes that are somewhat selective, and the outer membrane protects the cell wall. Because they lack a real cell wall, Gram-negative bacteria are more resistant to commonly used antibiotics. A different group of antibiotics is needed for these types of bacteria.
Mycoplasma spp do not have a cell wall; they only have a cell membrane, and grow very slowly, making them much more resistant to all known antibiotics. Mycoplasmas, specifically Mycoplasma bovis, is a highly contagious pathogen typically introduced when new animals are brought on the farm.
Selective treatment and selective dry cow therapy
Blanket dry cow therapy is now generally used in the US and other parts of the world. There is high social pressure on reducing antibiotics. The detection of specific pathogens can help with selective treatment of the animals.
These are the general recommendations, which vary by region and depend on the somatic cell count (SCC) in the bulk milk:
- Gram-positive bacteria: to be treated with antibiotics
- Gram-negative bacteria: not to be treated with antibiotics, because they are mostly cured easily after a few days
- Mycoplasma spp: separate or cull